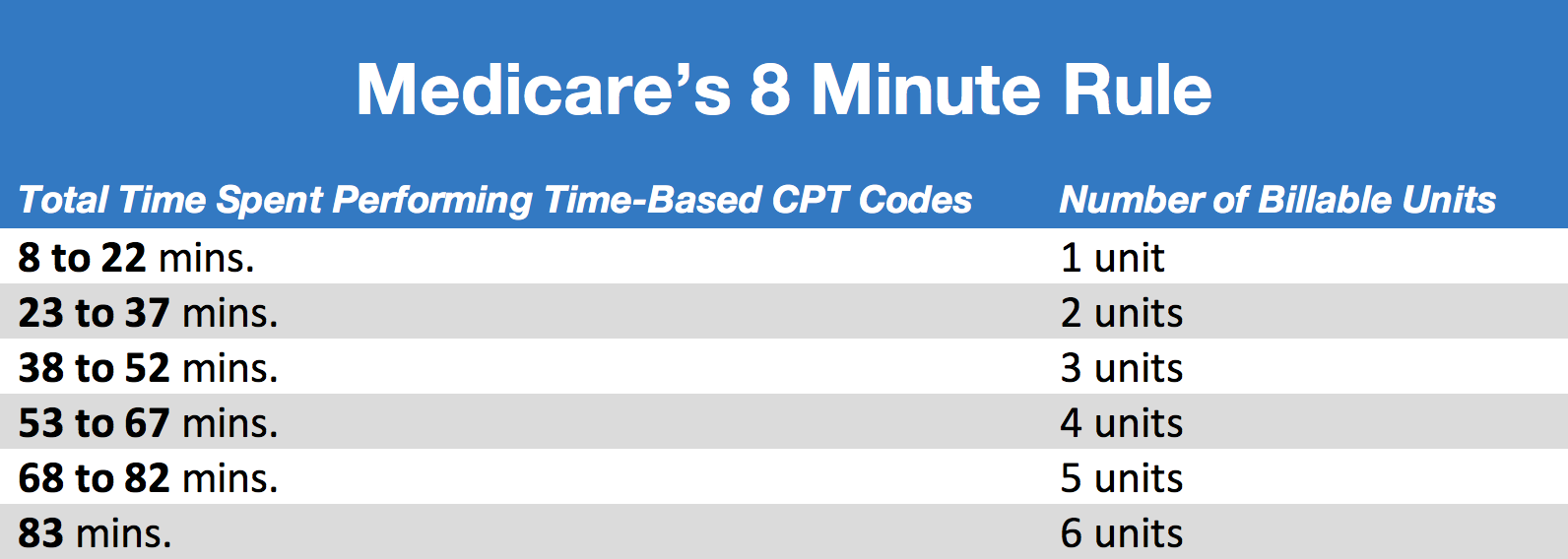
Medicare 8 Minute Rule Chart
Medicare 8 Minute Rule Chart - You can bill medicare for a single “billable unit” of service if it lasts at least eight minutes (up to 22 minutes). That's where this handy reference chart comes in. You must understand that billable units must equal at least 8 minutes of direct patient interaction for timed codes. This is an efficient way for physical therapists to bill medicare and figure out how many units they should bill for. Fact checked by ericka pingol. First, you need to add up the total treatment time for timed codes (do not include the time spent treating for untimed codes, only include time spent treating for timed codes). Web 8 minute rule chart. Web the 8 minute rule is a regulation set forth by medicare that states any service provided to a patient must be at least 8 minutes in length in order for it to be covered. If a service provided to a patient is not at least 8 minutes long, medicare will not provide coverage for it. Web at first glance, the medicare 8 minute rule seems fairly straightforward; Practitioners must spend at least 8 minutes on a service with a person before they can bill medicare. Web the 8 minute rule is a regulation set forth by medicare that states any service provided to a patient must be at least 8 minutes in length in order for it to be covered. For a service to be considered a. Web on the move: First, you need to add up the total treatment time for timed codes (do not include the time spent treating for untimed codes, only include time spent treating for timed codes). Web section 53107 of the bba of 2018 additionally requires cms, using a new modifier, to make payment at a reduced rate for physical therapy. The better medicare alliance has tapped rebecca buck to serve as its next senior vice president of communications. Anything less than that doesn’t qualify as billable time. It breaks down the specific guidelines for each therapy service, making it easier to determine the number of billable units. You must understand that billable units must equal at least 8 minutes of. Web the 8 minute rule is based on units of time, with each unit equating to 15 minutes. Web the rule allows practitioners to bill medicare for one unit of service if its length is at least eight minutes but less than 22 minutes. Web section 53107 of the bba of 2018 additionally requires cms, using a new modifier, to. So how do you know how many units to bill? Buck most recently served as senior director at the public affairs. Web at first glance, the medicare 8 minute rule seems fairly straightforward; For a service to be considered a single billable unit, it must last at least 8 minutes but not more than 22 minutes. That's where this handy. Web section 53107 of the bba of 2018 additionally requires cms, using a new modifier, to make payment at a reduced rate for physical therapy and occupational therapy services that are furnished in whole or in part by physical therapist assistants (ptas) and occupational therapy assistants (otas). Per medicare rules, in order to bill one unit of a timed cpt. Insurances that follow the 8 minute rule. Web 8 minute rule chart. This is an efficient way for physical therapists to bill medicare and figure out how many units they should bill for. Web you can bill for each individual code under the 8 minute rule. Find the total timed number of minutes on the right, and then get the. So how do you know how many units to bill? Web the rule allows practitioners to bill medicare for one unit of service if its length is at least eight minutes but less than 22 minutes. If a service provided to a patient is not at least 8 minutes long, medicare will not provide coverage for it. Web at first. Web section 53107 of the bba of 2018 additionally requires cms, using a new modifier, to make payment at a reduced rate for physical therapy and occupational therapy services that are furnished in whole or in part by physical therapist assistants (ptas) and occupational therapy assistants (otas). Web i could go on but you get the idea. Insurances that follow. Insurances that follow the 8 minute rule. Find the total timed number of minutes on the right, and then get the corresponding number of billable units on the left based on that time. Web handy 8 minute rule chart. So how do you know how many units to bill? Our comprehensive guide breaks down the rule with charts, examples, and. For a service to be considered a single billable unit, it must last at least 8 minutes but not more than 22 minutes. Find the total timed number of minutes on the right, and then get the corresponding number of billable units on the left based on that time. Web handy 8 minute rule chart. Treatments are billed to medicare in units, and treatment must last no less than 8 minutes for a unit to be billed to medicare. If a service provided to a patient is not at least 8 minutes long, medicare will not provide coverage for it. Therefore, for a service to be billable, it must be provided for at least half of the unit time, i.e., 8 minutes. This is an efficient way for physical therapists to bill medicare and figure out how many units they should bill for. Insurances that follow the 8 minute rule. Web the 8 minute rule is a regulation set forth by medicare that states any service provided to a patient must be at least 8 minutes in length in order for it to be covered. It breaks down the specific guidelines for each therapy service, making it easier to determine the number of billable units. Web at first glance, the medicare 8 minute rule seems fairly straightforward; Web the rule allows practitioners to bill medicare for one unit of service if its length is at least eight minutes but less than 22 minutes. Practitioners must spend at least 8 minutes on a service with a person before they can bill medicare. The rule states that a rehab therapist healthcare provider must provide at least 8 minutes of physical therapy services to bill for one unit of that service. Web on the move: Web you can bill for each individual code under the 8 minute rule.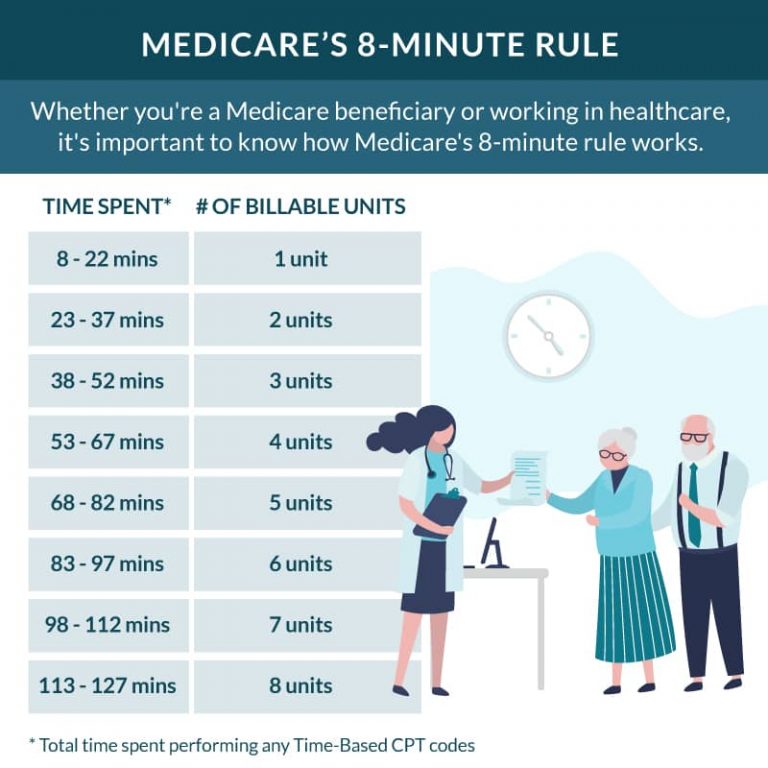
Medicare's 8Minute Rule A Comprehensive Guide
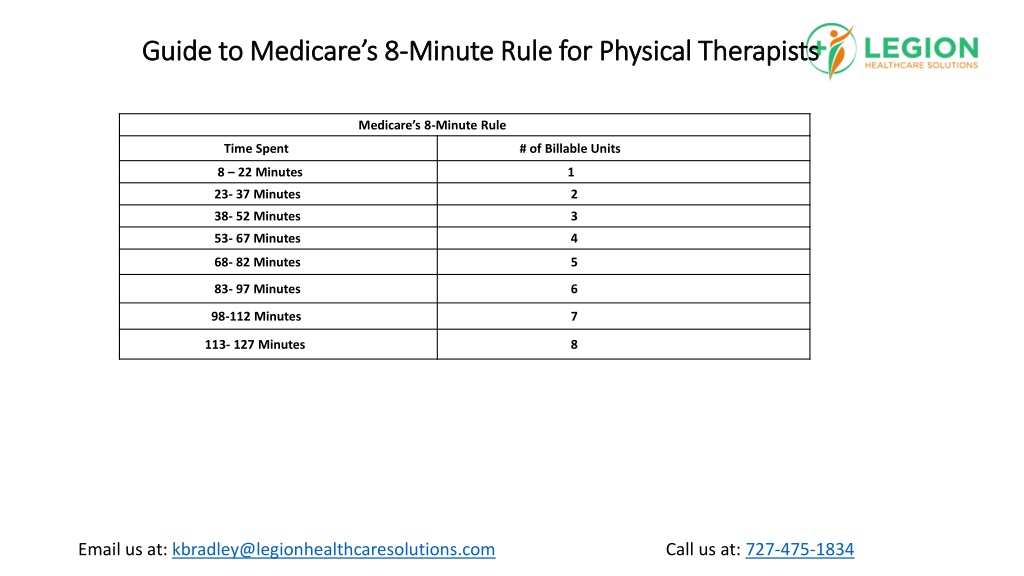
PPT Guide to Medicare’s 8Minute Rule for Physical Therapists
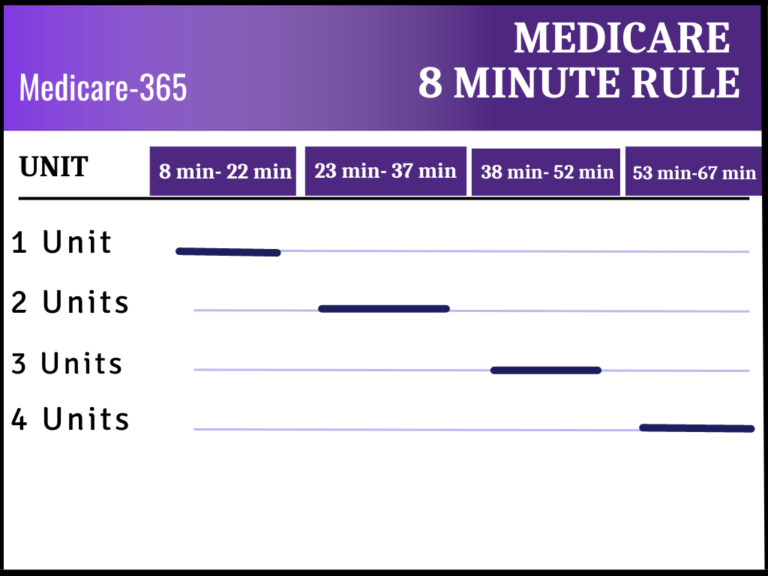
Medicare 8 Minute Rule Medicare365
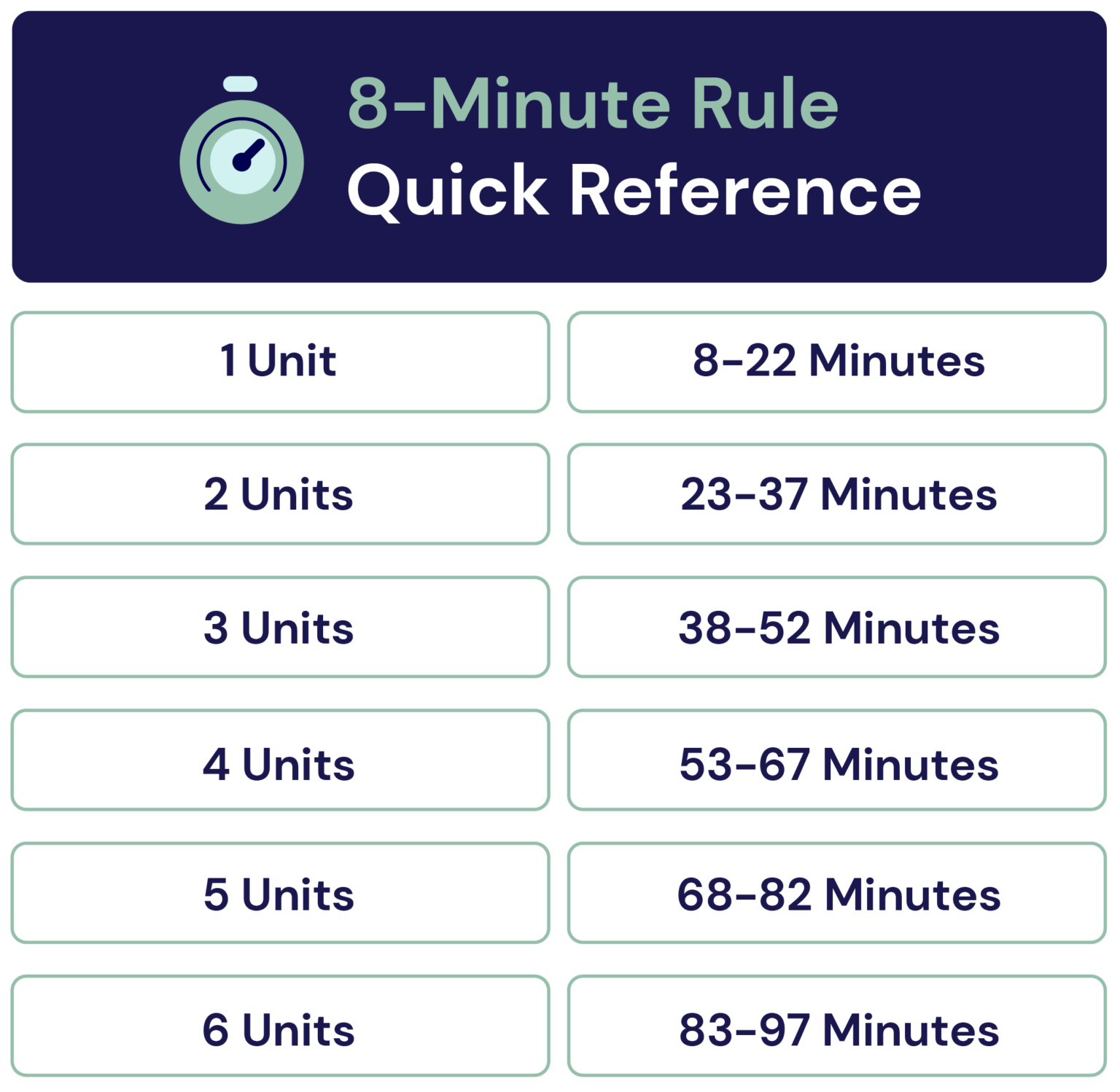
A complete guide to the Medicare 8minute rule. Clinicient

Medicare 8 Minute Rule Chart

Medicare’s 8Minute Rule What It Means for You CoverRight
How Medicare's 8Minute Rule Works Practice Perfect

Medicare 8 Min Chart

Medicare 8Minute Rule Senior HealthCare Solutions

Medicare's 8Min Rule Explained Key Insights & Tips The Medicare Family
Web 8 Minute Rule Chart.
You Can Bill Medicare For A Single “Billable Unit” Of Service If It Lasts At Least Eight Minutes (Up To 22 Minutes).
Suppose You Performed 3 Different Treatments, But Only Spent 5 Minutes On Each One.
Web The 8 Minute Rule Is Based On Units Of Time, With Each Unit Equating To 15 Minutes.
Related Post: